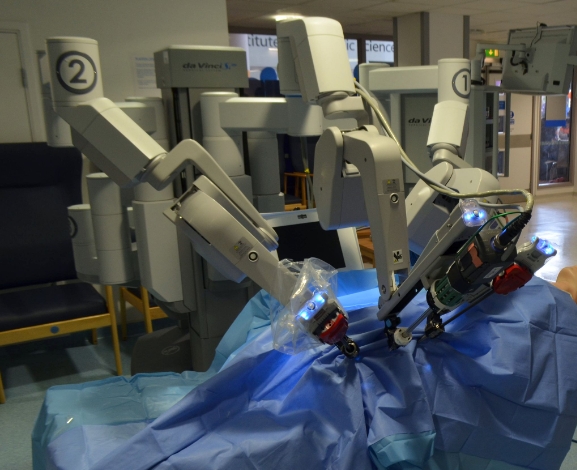
Days before S.I.U.T a renowned non-profit hospital in Pakistan started complete automated surgery operations through robots. This is an immense milestone in transforming digital healthcare in countries like Pakistan where free health caring opportunities were always an issue, because of vast budget involvement owing to grappling economic conditions, the provision of basic healthcare is a huge challenge. This dare for rising medical budget costs lies not only with third world countries but also developed and higher GDP ratio economies like the US, UK, and other European countries that are scuffling with these issues.
Healthcare in today’s world is under extreme challenges to not only survive under immense business environments worldwide but also to up bring new innovations. These innovations like Digital Data Optimization, Evolving
Business EcoSystems, and the Implementation of biosciences based Artificial
Intelleingce are changing the human age not only in other business but also in healthcare where no. of specializing professionals works under one medical institution and other government and private organizations.
Digitally Evolving HealthCare Ecosystems:
Over the past year, post-pandemic, the healthcare sector experienced a dramatic change in requirements for speeding up the non-productive processes, which led them to transform themselves into digital records of health consumers and their medical history, now need to connect more records to the healthcare ecosystem for intense data analysis and for better patient care. Because of strict regulations and the desire to avoid unintended harm new technology, research, and clinical trials are often rigorously tested and adopted gradually. This sometimes makes this approach so lengthy that researchers and biological data analysts feel so hard to integrate the innovations and inaccessible in real-time.
Understanding the Digital HealthCare Ecosystems:
Mainly many healthcare consultations require in-person care but the pandemic has changed the way to virtual care and remote patient monitoring, for example, Hospitals experience providing rapid medical offering 100% more via telehealth options in covid time which generates the need for pharmaceutical and Medtech industries to emphasis on digital scanning of the medical history of consumers for
better consultations. Adaptation to this process led medical practitioners to change their operational mindset and to gather their focus on the more problematic issues of healthcare consumers rapidly.
From
the organization-centered healthcare model to the patient-centered model, this
system allows healthcare professionals to examine virtual health records (VHR)
for a 360-degree view of patient conditions and enables multiple care systems
to work in collaboration for better services.
Business Under Technology & Innovation:
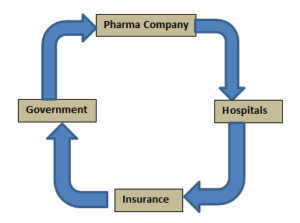
First, we have to understand how healthcare circular financing works in pharmaceutical and healthcare systems, governments, and manufacturing companies.
Consumer Ease-Based Model:
Empowering customers to plan and maintain their healthcare plans can be achieved through economical insurance plans which can give them greater control over their health life spending. They eventually not only want advanced technology of good quality and at a good speed to ease their process. The existing traditional system engages people on a pro long waiting list for their checkup and afterward referred them from one facility to another for crucial disease stages which involves no. of medical disciplines.
Healthcare is a fragmented industry where investors and venture capitalists term investment at immense risk assessment. A money roller can take returns from an IT sector in planned time as per feasibility but in health care times it took them to see maturity or even approval of a product after 10 years.
Researchers segregated invocation into two categories, where one can roll a no. of independent medical practitioners into a single organization called horizontal integration, or we can develop infrastructure for the treatment of a chronic disease under one roof which is called vertical integration. From this patients get on stop shopping and are freed from dealing with different practitioners separately.
Influenced By Stakeholders:
The Healthcare industry has always been influenced by no. of stakeholders whose stakes aren’t always the same for each product and shifting policies. Often, they have substantial resources and power to influence public policy or opinion by enforcing their agenda on innovators. For example, hospital staff, doctors, and administration sometimes blame technology for high-cost treatments. Public leaders and policymakers have their own agenda to implement and show sympathy for public fame and votes. Thus, influencing the right policy or better business model has always been a problem for ease in processes.
Improving Finance Models:
The major problem is the long time investment needed for new drugs, systems, or therapies that require the medical body’s approval. Another problem is that traditional resources of capital aren’t familiar with healthcare so challenges are real: who will pay or how much for the prototype product before clinical trials. A single resource investor problem is the confusion about complex reimbursement and payments system which finally comes from the third-party insurer or Government. Relationships in regularising the funding plays a vital role, an insurance firm that is scaling its growth from annual turnovers usually takes incentives, discounts from medical companies, and healthcare setups to promote new advanced products for more clinical practices. Practically doctors may oppose new innovations such as implant monitoring devices which may affect their fee for the same diagnosis.
Audit Policies:
In today’s age thanks to technology and on-hand search facilities, customers are empowered and they ask policymakers to tighten their noose at medical companies to implement safety in their innovations. But most of the processes led by the researchers approved by companies for clinical trials or even after the government’s approval, have intentions to increase the frequency of process and revenue rather than results and their accuracy. To prevent this and ensure safety in health diagnosis audit and compliance with the policy is necessary, which will enforce practitioners to avoid any malpractice by machines and their new technology.
Changing The Mindset:
Consumers generally are not willing to pay for conventional healthcare facilities, they would never resist before buying a $20,000 New Model Car but will hesitate to do a $1000 image scan for their lives, this led consumers to fear that they might be spending more money for a faulty or diagnosed image. We need to rethink our mentality and approach to spending our money, as health will pay off in the end. Insurers have also their part in running this finance system as they are rather possessive about the process to create revenue from After services of equipment consuming their maintenance life cycle.
Many companies in the past tries to set up the business finance model on a non-insurance low-cost process system but eventually failed to survive after some years because of various reasons. Some found their customer acquisition cost too high, and some were bad-mouthed by doctors and practitioners for their non-hospitalization business model by enabling their clinical system less equipped with emergency trials.
Capital Cost Cover-up:
Innovators should keep in view, the long-term beneficiary relationships between them and the network e.g. distributors and insurers. For example, generally, insurers do not pay separately for capital equipment so the hospital expense must include a fraction of their expenses to cover the capital cost which is always on the higher side. In this case vendor of a new advance, the CT Scan camera machine covers the capital cost from the insurer’s bills.
Sometimes the capital cost for installation, operations, and continuous software development during the process is so high that capital ventures, Healthcare firms become exhausted to refuel it with major developments. So if the installed site and equipment manufacturing destination is identical, maintenance cost lies within the budget but for third world countries, and African nations where Healthcare is always been a challenge, maintenance budget sometimes exceeds to throw the new developments out of the list.
Regulations for Non-Profit Organizations:
Only legislators can re-regulate the policies to eliminate obstacles in the provision of better healthcare especially covering Non-Profit organizations, though audit and scrutinizing of these organizations is always been a question to make utilization of funds 100% effective these ventures are the ones struggling to provide the latest healthcare facilities to needy consumers, especially in countries with lower GDPs.
The question is also to remodeling these healthcare providers as a non-profit organization mostly follows horizontal integration models where they are dependent on no. of different discipline practitioners which led them to always begging for their finances because applying vertical integration to their working requires huge capital costs which seems unaffordable for them. But Governments should work on policies to fund these organizations for vertical integration models where treatment can be possible for most chronic disease patients.
Conclusion:
The substructure described in this article is just to present some ideas with possible obstacles to engaging more technology and innovation in healthcare systems. Many firms have now transit them into new modern AI-based software models but most of them especially in underdeveloped countries are still struggling to maintain cost control and profits for running their expenses.
Governments can rework the old house traditional policies to replace them with new cost-effective and more expanded consumer side models so that quality health services, emergency identified and more diagnostic services can be offered and prevail in the confidence of venture capitalists, investment firms, and single-headed investors to inject more capital into healthcare for making the world better place.